
Increased Revenue: Improved documentation accuracy can lead to more accurate coding and billing, which can increase revenue and reduce the risk of denials and audits.īetter Compliance: A good CDI program can help ensure compliance with regulatory requirements, such as coding and documentation guidelines, and reduce the risk of penalties and fines.Įnhanced Efficiency: Accurate and complete documentation can help streamline workflows and reduce administrative burden, freeing up healthcare providers to focus on patient care.
Improved Quality of Care: Accurate and complete clinical documentation can help ensure that patients receive appropriate and effective care based on their individual needs, which can improve patient outcomes and satisfaction.
Overall, a good CDI program can help improve the quality and safety of patient care, increase revenue, reduce compliance risks, enhance efficiency, and support population health management efforts, benefitting both inpatient and outpatient facilities.Ī good Clinical Documentation Improvement (CDI) program can have a significant impact on both inpatient and outpatient facilities, including: Improved population health management: CDI can help support population health management efforts by ensuring that documentation accurately reflects the health status of the patient population, which can be used to identify and address gaps in care and improve outcomes.

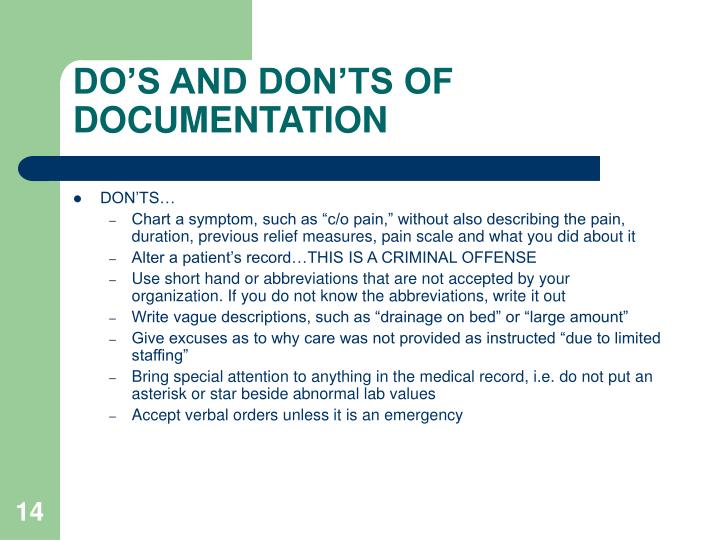
Increased revenue: Improved documentation accuracy can lead to more accurate coding and billing, which can increase revenue and reduce the risk of denials and audits.īetter compliance: A good CDI program can help ensure compliance with regulatory requirements, such as coding and documentation guidelines, and reduce the risk of penalties and fines.Įnhanced efficiency: Accurate and complete documentation can help streamline workflows and reduce administrative burden, freeing up healthcare providers to focus on patient care. Improved quality of care: Accurate and complete clinical documentation can help ensure that patients receive appropriate and effective care based on their individual needs, which can improve patient outcomes and satisfaction. CDI can help support population health management efforts by ensuring that documentation accurately reflects the health status of the patient population, which can be used to identify and address gaps in care and improve outcomes.įinally, the widespread adoption of electronic health records (EHRs) has made it easier to capture and analyze patient data in outpatient settings, providing opportunities for CDI to leverage technology to improve documentation and enhance the quality of care.Ī good CDI (Clinical Documentation Improvement) program can have significant positive impacts on both inpatient and outpatient facilities, including: CDI can play a critical role in ensuring that outpatient documentation is accurate, complete, and supports the care provided.Īnother initiative is the increasing focus on population health management, which involves managing the health of a defined patient population across the continuum of care, including in outpatient settings. These models incentivize healthcare providers to improve the quality of care and reduce costs, which requires accurate and complete documentation of patient conditions and treatments. One of the key initiatives is the shift towards value-based care and alternative payment models, such as accountable care organizations (ACOs) and bundled payments. There are several initiatives that are promoting the expansion of CDI (Clinical Documentation Improvement) into the outpatient settings.


 0 kommentar(er)
0 kommentar(er)
